Information & inspiration
modern claims management
Discover articles, white papers, case studies, and tools that help you make your claims process smarter and more transparent.

What we stand for
Four pillars that make your organization ready for growth and innovation.

Transparency
Real-time insight for management, teams, and customers.

Automation
Smart workflows ensure speed and precision.

Integration
Connects all systems and partners without replacement projects.

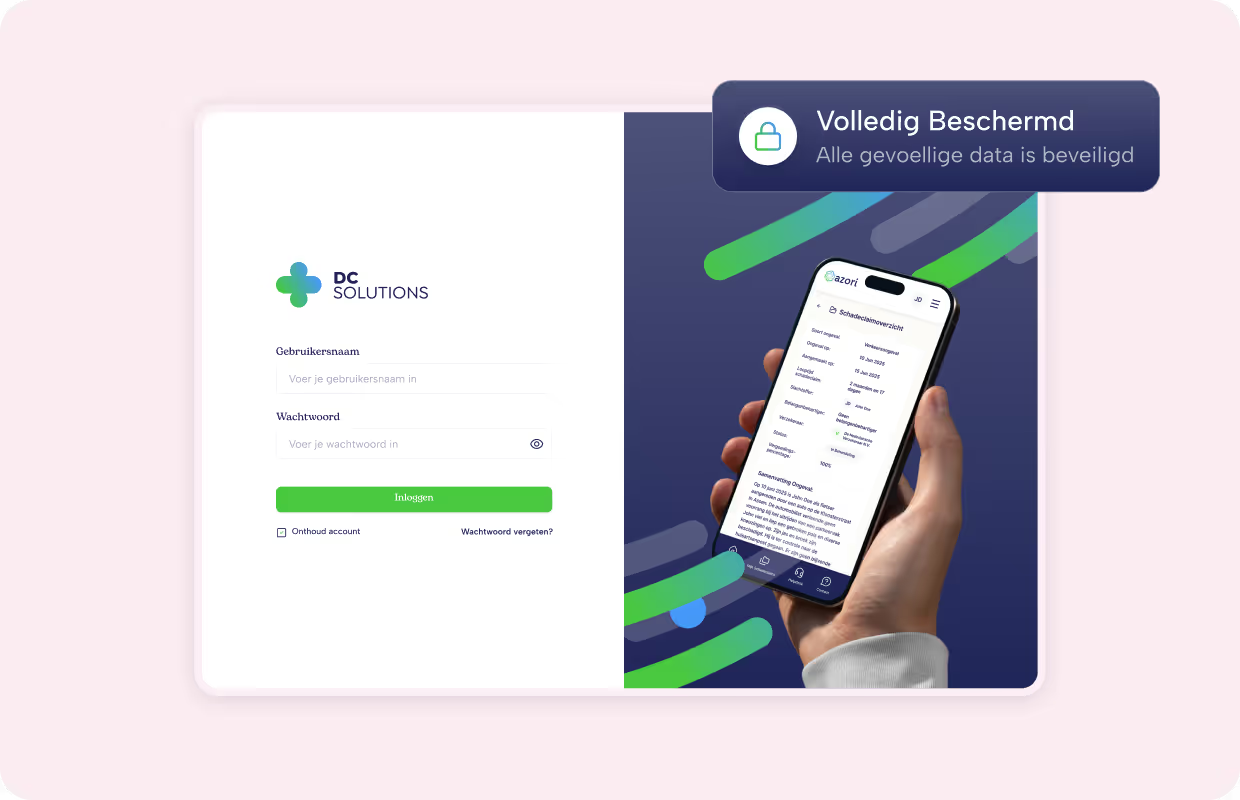
Safety
Fully GDPR-compliant and ISO 27001 certified.

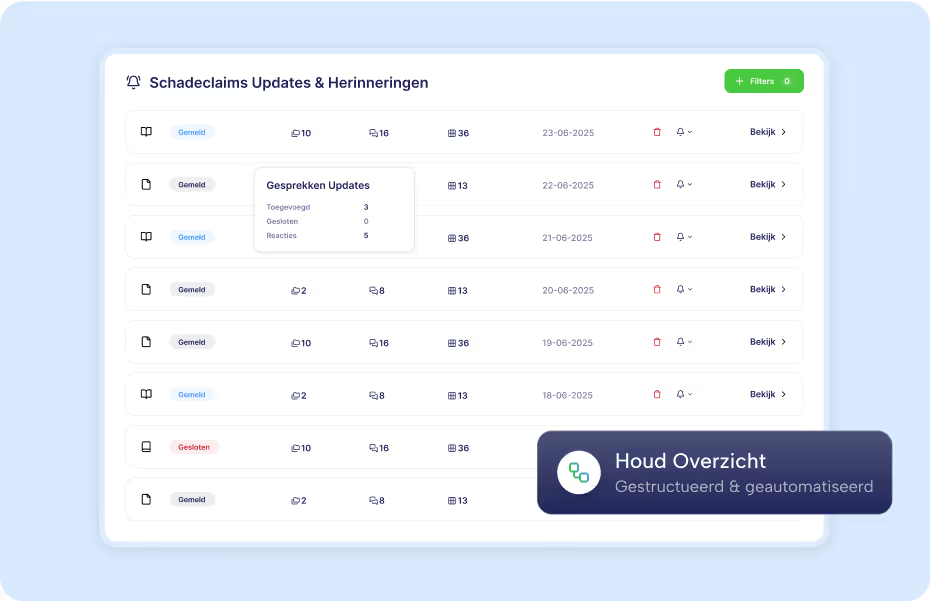
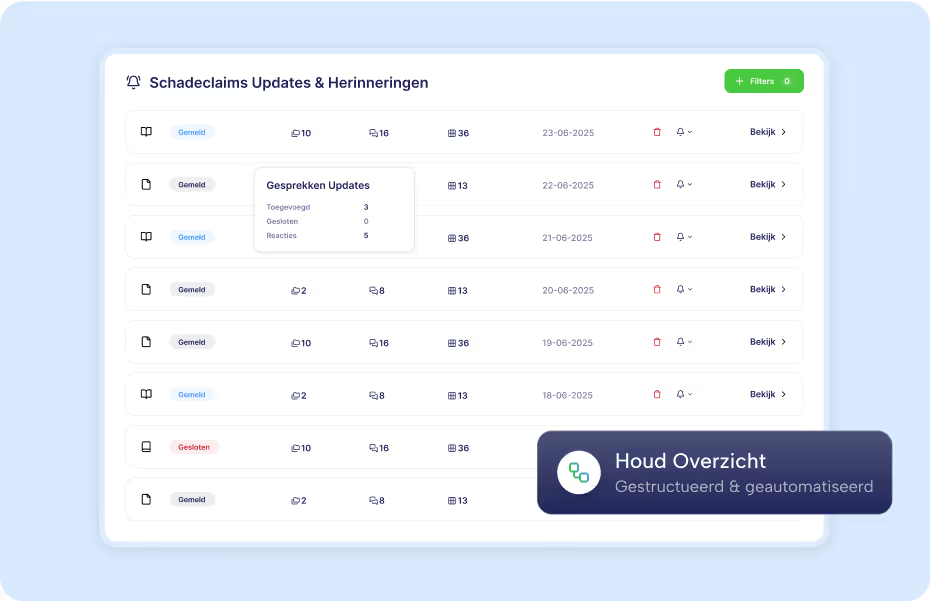
Transparency for everyone in the process
Insured persons, service providers and internal teams work together in one environment.
- 24/7 insight into status and progress.
- Securely share documents and data.
- Clear roles and rights, so that everyone sees exactly what is relevant.

Automate where possible, escalate where necessary
Leave repetitive tasks to smart workflows and ensure that complex cases get the right attention.
- 24/7 insight into status and progress.
- Securely share documents and data.
- Clear roles and rights, so that everyone sees exactly what is relevant.

Connect everything without replacement projects
Integrate effortlessly with existing policy and claims systems. Our API-first architecture makes connections simple and scalable.
- 24/7 insight into status and progress.
- Securely share documents and data.
- Clear roles and rights, so that everyone sees exactly what is relevant.

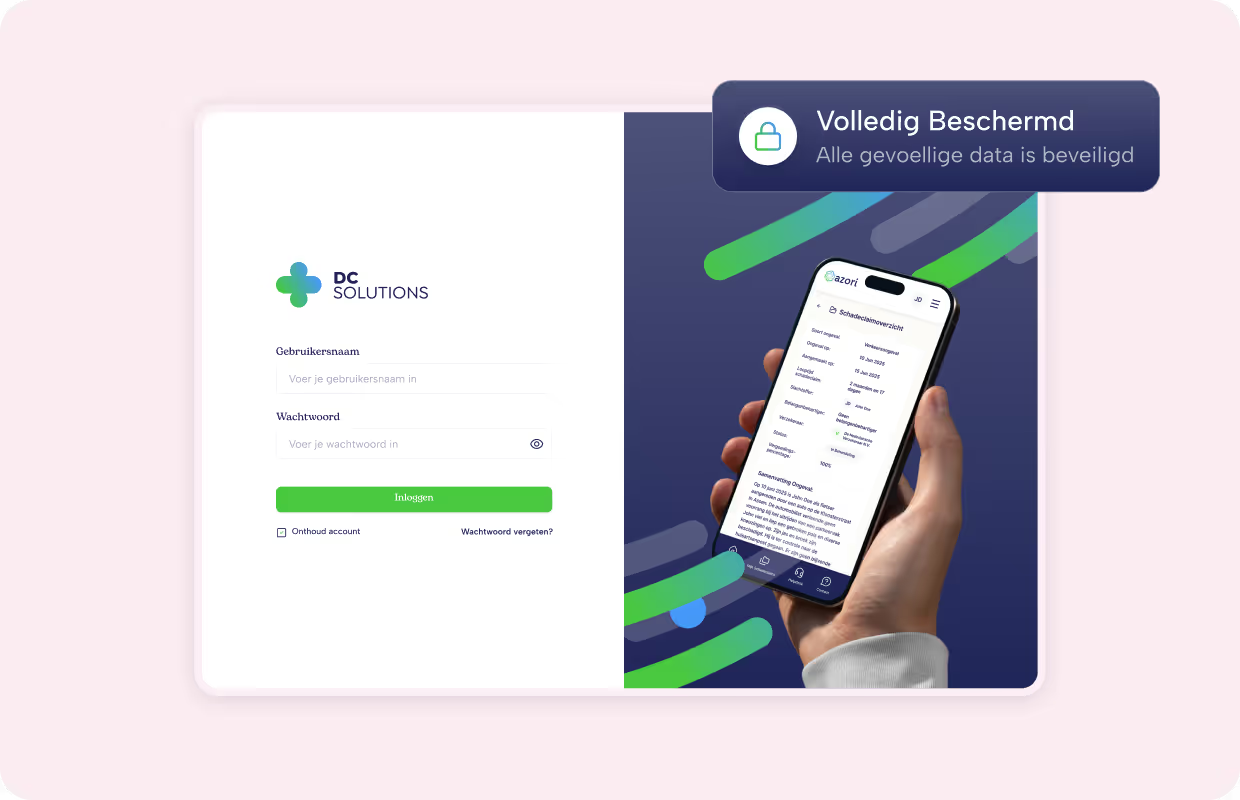
Protect sensitive data today and tomorrow
Our solution meets the highest standards of safety and compliance.
- 24/7 insight into status and progress.
- Securely share documents and data.
- Clear roles and rights, so that everyone sees exactly what is relevant.
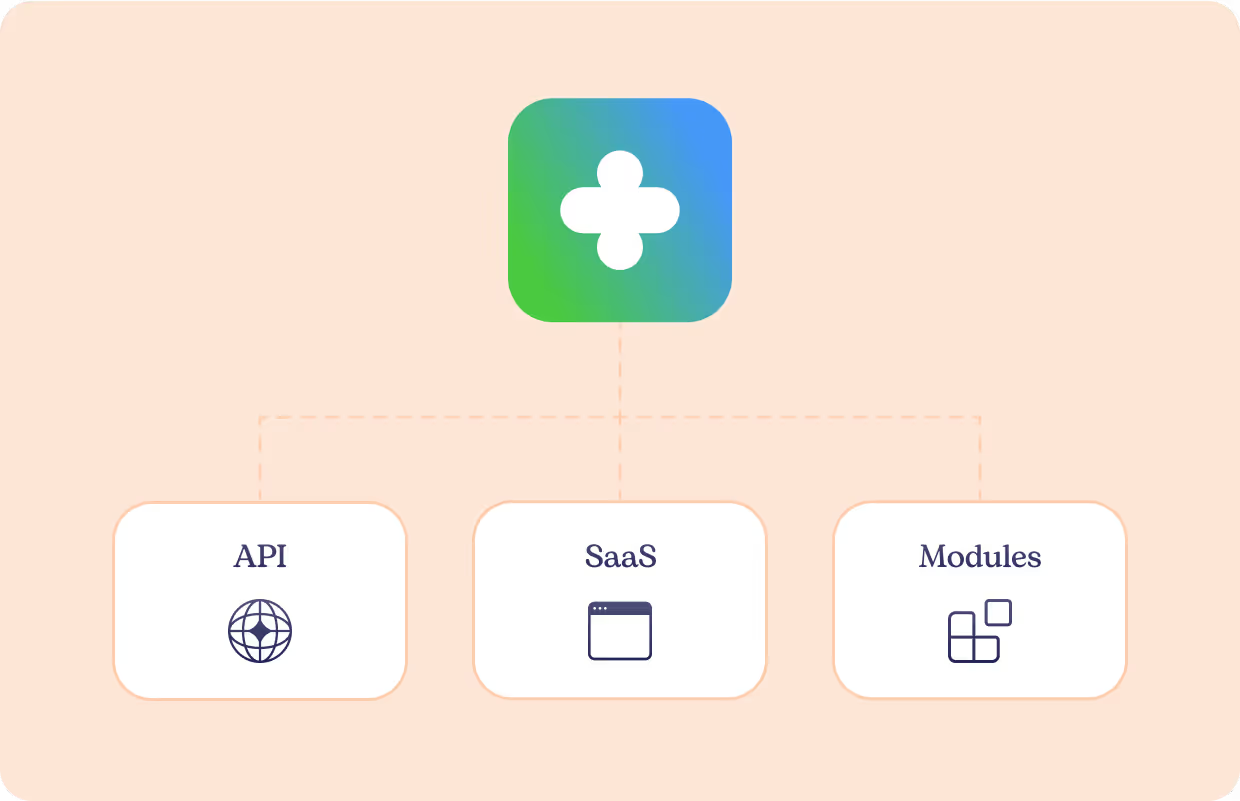
Our products and services
Handle claims faster, smarter and more transparently together.
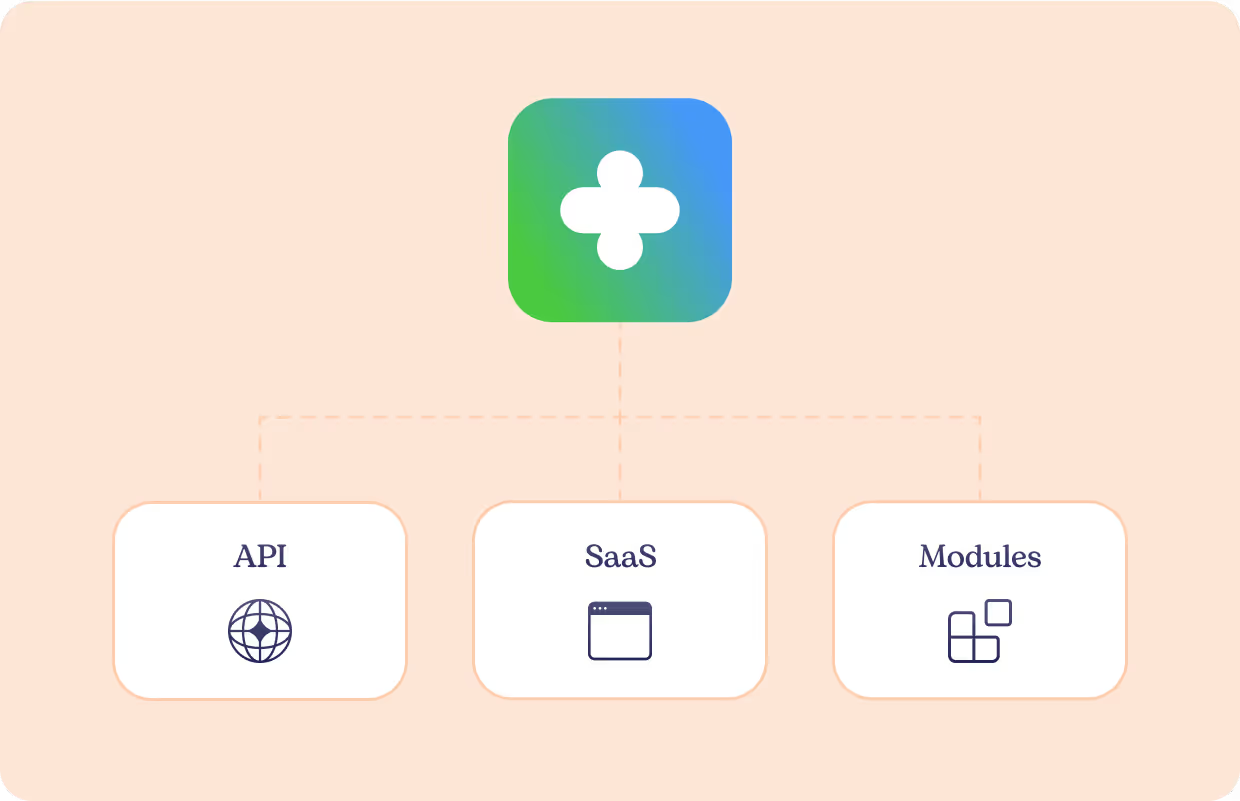
Claim 360
Claims distribution platform

Claim360 is designed for the standardized exchange of claim information with all parties involved in the claims ecosystem. Thanks to its API-first architecture, Claim360 easily connects to policy and claims systems, including legacy, and ensures secure, real-time information exchange. In doing so, it acts as the engine for uniform claims handling, regardless of the systems used or chain partners.
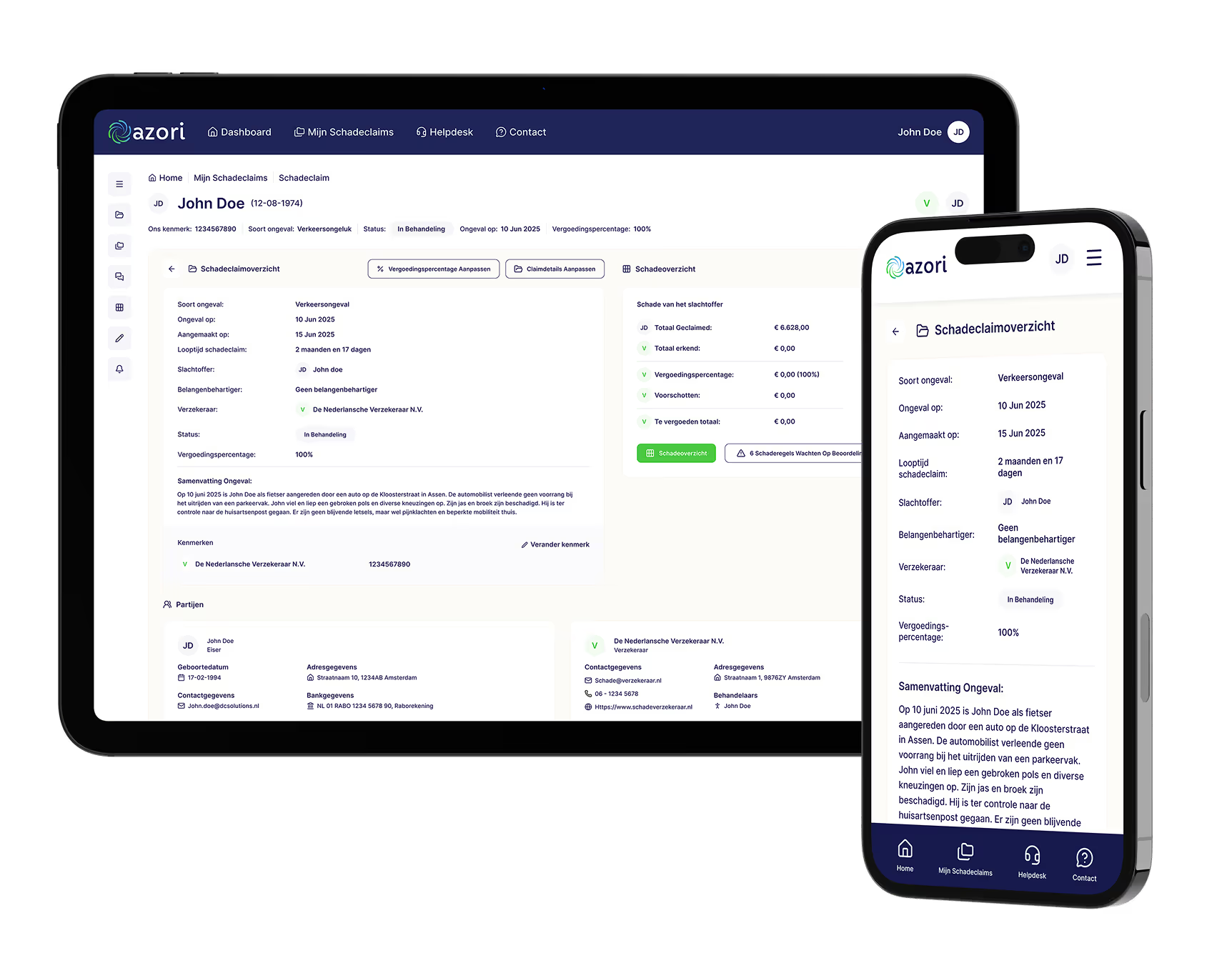
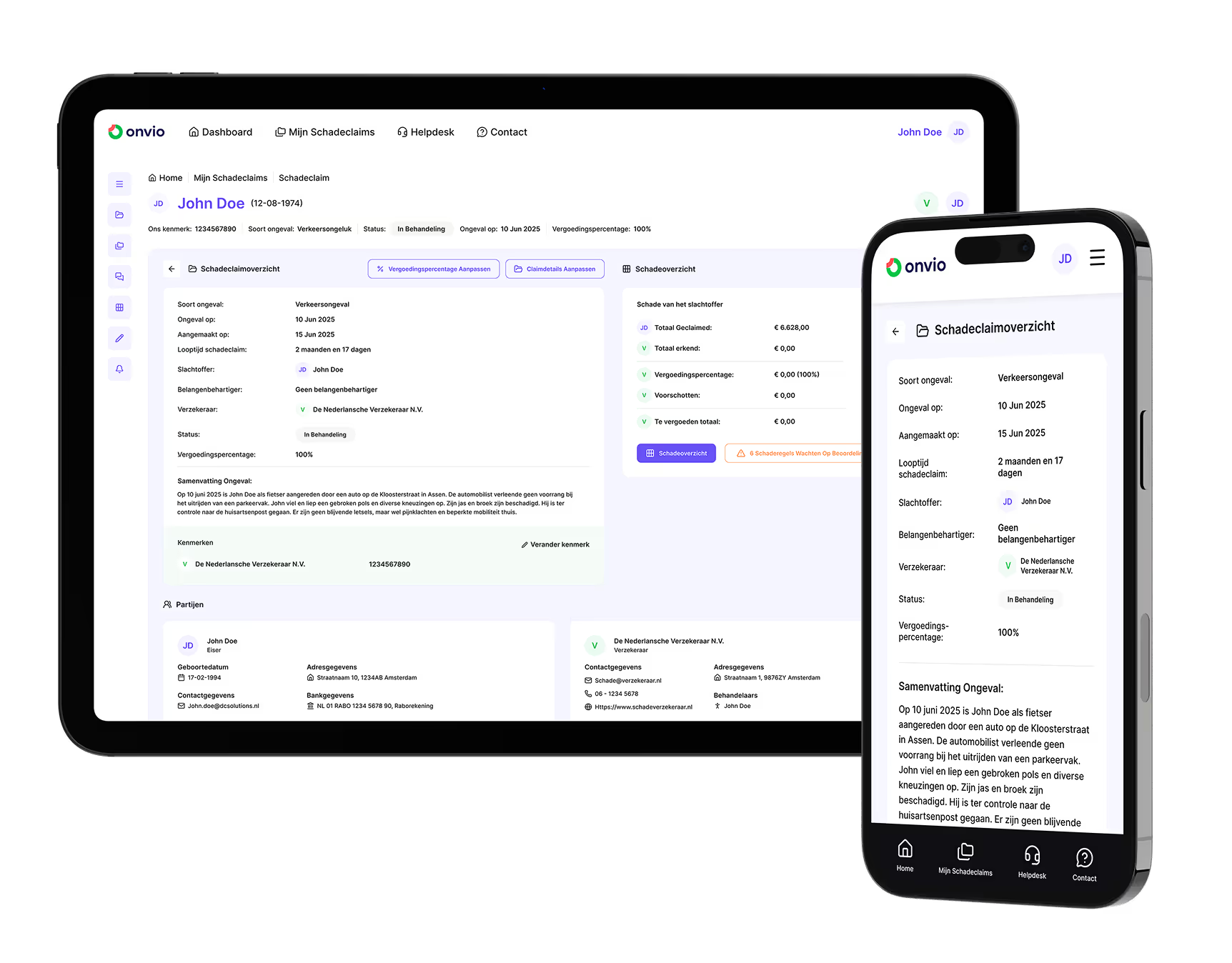
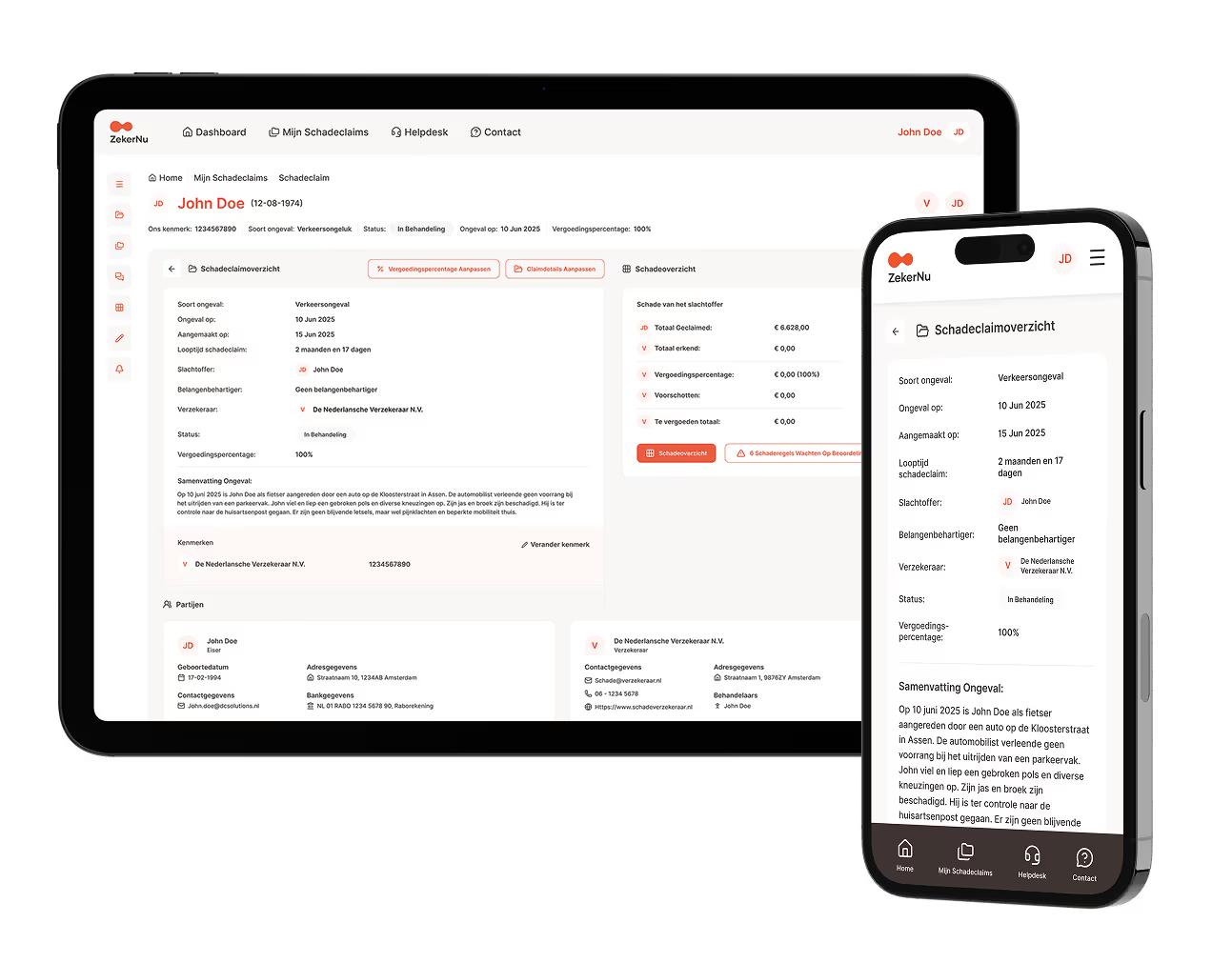
Azori
SaaS user interface

Azori is the SaaS graphical operating environment on top of Claim360. This service can be used white-label in the organization's own corporate identity, so that all parties in the claim process work together within one uniform environment. Azori provides a consistent user experience for customers, claimants, advocates, claims adjusters, and chain partners. Claim information, files and conversations are bundled here, with a direct link to the underlying systems, ensuring transparency, ease of use and efficiency.
Solution Hub
Accelerating building blocks

Solution-Hub consists of ready-to-use building blocks, such as intake, assessment, communication and reporting. These components are proven in practice and can largely be deployed immediately: the rule is that 80% of the work is already done, and only 20% coordination is needed to make them seamlessly connect to an organization's specific processes. In this way, Solution-Hub accelerates implementation and leaves room for customization. The building blocks connect flexibly to existing systems and form a solid basis for further expansion.
Customization
Where standard is not enough

When standard is not enough, we develop solutions based on Claim360 that exactly meet unique needs. These integrate seamlessly into the existing landscape and can be flexibly expanded for future needs.
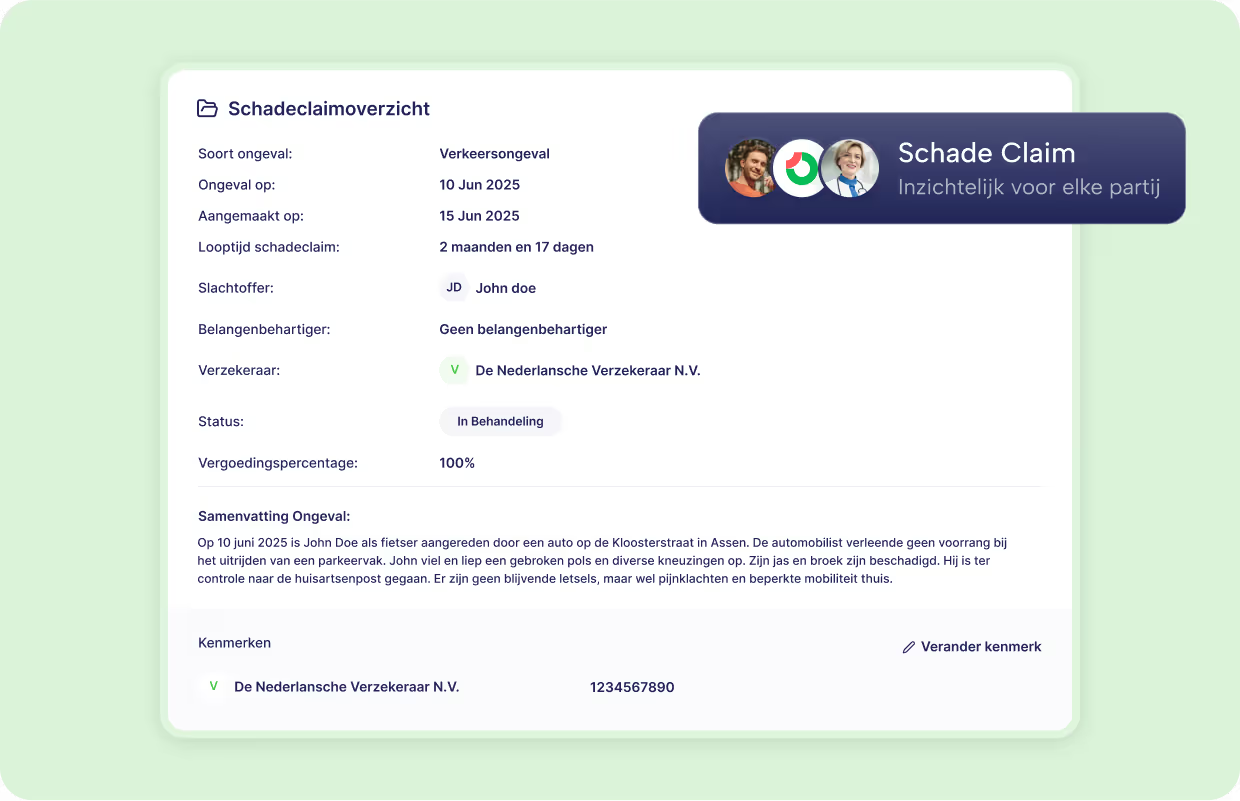
One ecosystem, tailored to each user
Our platform offers everyone involved an environment that exactly matches their role. This way, everyone works together efficiently, while all data is synchronized in one central system.
Simple and clear insight for customers and clients
Insured persons get direct access to their claims via the portal and can easily manage documents, reports and communication.
- Report and track damage quickly
- Secure document exchange
- Transparent process without noise

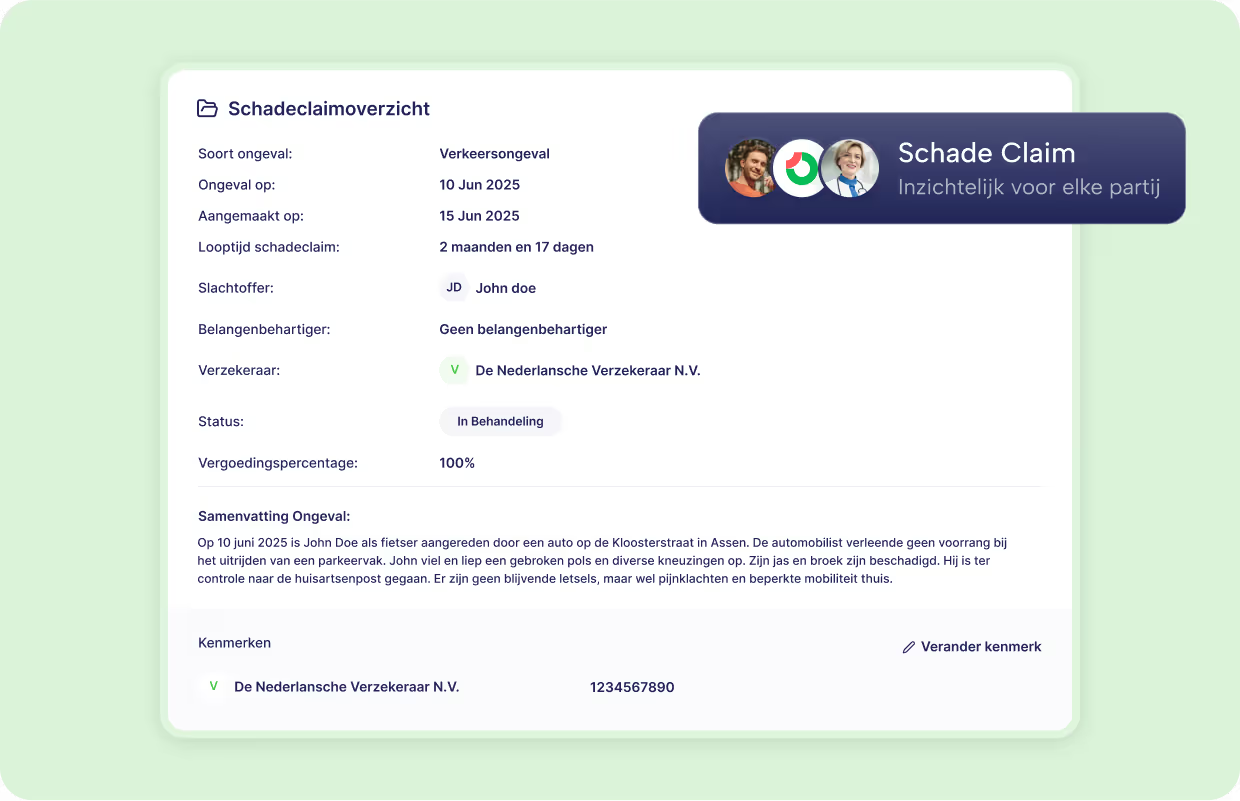
Full transparency and empathy during the claims process
Through a user-friendly portal, claimants always have insight into their file, so that they know what steps are being taken and where they stand.
- Always insight into status and progress
- Clear updates and communication
- More trust and control in the process

Efficient work processes for therapists and claims experts
All files, tasks and workflows come together in one clear environment, while complex rules are applied automatically and error-free.
- Clear tasks and priorities
- Smart workflows for faster processing
- Less manual work and errors

Real-time collaboration without separate emails or spreadsheets
Service providers receive direct access to relevant files and tasks via a dedicated portal, such as Azori.
- Always up to date information and deadlines
- Secure data sharing (GDPR-compliant)
- Less delay and miscommunication

Real-time insight for better decisions and continuous improvement
With dashboards and reports, management has full control over performance and bottlenecks in the chain.
- Dashboards with current KPIs
- Insight into bottlenecks and trends
- Strategic process improvement




